If you’ve landed here, you are likely one of the millions of Australians who live with irritable bowel syndrome (IBS) and are looking to improve their gut health with an IBS nutrition plan. Having a history of IBS myself and choosing my career path as a Nutritionist and Naturopath thanks to the successes I had experienced through dietary and naturopathic treatments; I understand whole-heartedly the impact IBS can have on your life.

Your Tests are Normal, but Your Symptoms are Definitely NOT!
You’ve been to the GP, had blood tests, stool tests and a colonoscopy, yet, by the end of it all you are told is, “everything looks normal”. Sounding familiar? With symptoms like bloating, constipation, diarrhoea and abdominal pain, you know within yourself it is anything BUT normal.
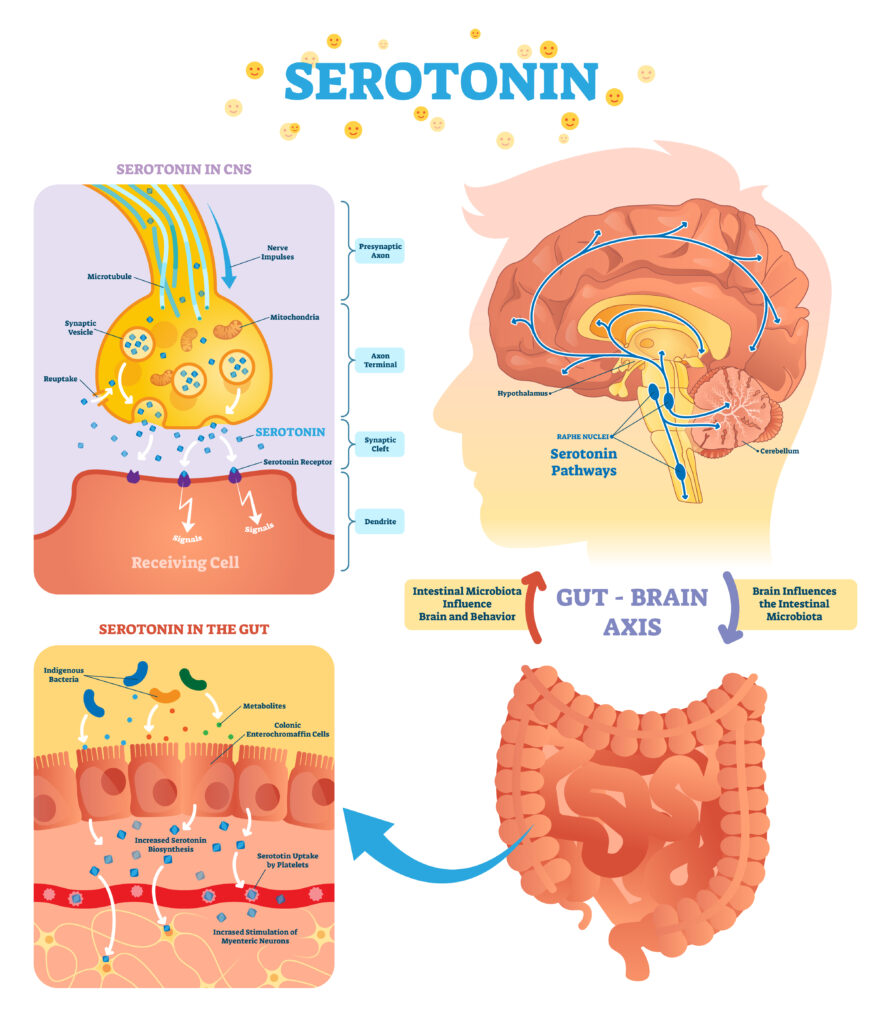
Because IBS is a functional disorder, rather than a structural disorder, abnormalities do not show up on regular tests. Despite this, I can assure you, your symptoms are very real. IBS is greatly affected by your emotional wellbeing. The interaction is referred to as the gut-brain axis. This very clever and connected system houses an entire nervous system, including the vagal nerve. Further, stress hormones such as cortisol and neurotransmitters such as serotonin (the happy hormone) function within the gut-brain axis. When you are stressed, this interaction becomes overstimulated and gut function is impacted, resulting in IBS symptoms.
You may also experience increased or decrease motility (movement of stool through the bowels), with visceral hypersensitivity (discomfort/pain). These factors can make normal digestive processes uncomfortable. When you pair stress and this hypersensitivity together, you get unpleasant nerve signaling, imbalances in gut bacteria and bloating.
A Gutful of IBS
IBS is one of those frustrating conditions that can feel like everything you eat is causing bloating or exacerbating your constipation or diarrhoea. You become scared to eat out and are constantly thinking about where the closest toilet is. You become so bloated, you look 6 months pregnant. I can imagine you nodding your head along as you read those words. Yes, I get it. 13 years ago, I was right there with you, suffering through the embarrassment, the discomfort, the frustration and the fear of eating.
Fast forward to my first year of my nutrition degree. I learned how to reduce the inflammation in my gut, balance gut bacteria, heal up the lining of the gut to reduce ‘leakiness’ and, formulate an IBS nutrition plan that worked for ME.
We then fast forward another 3 years to my final year in Nutrition Clinic. Here, I see patients and start applying what I learned over the years to the various types of IBS presentations in individual patients. Let me tell you, no two treatments were the same.
IBS treatments and their responses vary from person to person. Many people who have IBS, their triggers can be as different as night and day. As can their symptoms.
Some people may have IBS – D where they experience more diarrhoea. Others experience IBS – C which is constipation dominant. Then there are those who experience a combination of the two. Some can be triggered by anxiety and depression. When you consider the well-researched Gut-Brain Axis and the fact that neurotransmitters that affect our happiness are largely produced in the gut, it is no wonder anxiety and depression play major roles in gut function.
Bloating and Diet
Bloating is one of the most common symptoms of IBS. Changes to the diet can significantly improve bloating and digestive discomfort.
This uncomfortable symptom can be triggered by several factors including:
- fermentable carbohydrates (FODMAPs)
- food intolerances
- carbonated drinks
- artificial sweeteners
- hormones and stress
Bloating and diet go hand in hand, just as the reduction of bloating and the diet go hand in hand. A plan to reduce bloating may include but is not limited to :
- a careful balance of nutrients
- meal spacing
- vagal nerve stimulation
- ensuring mechanical processes such as chewing are effective
What does an IBS Nutrition Plan involve?
When considering the treatment of a patient’s IBS symptoms with nutrition, there is more to it than simply providing a generic list of what ‘to’ and what ‘not to’ eat. As previously mentioned, each case of IBS is different. Not just the physical symptoms but also the individual foods and food compounds that people react to varies. To support the development of the best strategy for your individual needs, an in depth analysis of the following are required:
- your food diary
- patterns in symptoms
- identified and possible triggers
- your lifestyle
Low Fodmap Coaching and IBS Nutrition Plans
Low Fodmap is a bit of a buzz in the IBS space, and we are seeing an increasing number of new food products hitting the shelves claiming to be Low Fodmap. Just like the gluten-free craze, this is great for those who have a true IBS picture to start somewhere. However, a Fodmap protocol is a process that requires careful and guided implementation, by a qualified dietary professional, with experience in this area.
Cutting out large food groups and nutrients for any length of time can be detrimental in the long term, creating nutrient gaps. I too often see people completely avoiding dietary fibre sources which can further limit digestive function.
There are different types of Fodmap foods, and not all types affect every person with IBS. For the sake of keeping this blog post short and sweet, the simplest explanation is, Fodmap requires a distinctive process of elimination, rechallenge and personalisation using a stepped strategy. Focusing on balancing nutrients and re-establishing the gut lining and the microbiome form part of your treatment protocol. Low Fodmap Diet and elimination strategies clearly identify the triggers of IBS symptoms, but are not implemented long term by practitioners.
As you can see, the treatment of IBS with an effective, individualized and targeted nutrition plan with a dietary strategy suited to you and your symptom presentation, while improving long term gut function is the key to effective results. Whether it be Low Fodmap Coaching, gut supportive supplementation or making smaller tweaks to the diet a personalised approach is the only approach to IBS.

